By Jon Cohen
Feb. 24, 2016 , 10:45 AM
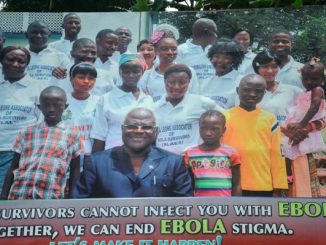
Bernadette Jebessaoy and her mother, Ioye Massaquoy, survived Ebola. A study has found that 83% of patients had at least one long-lasting symptom from the virus.
Zika may be the virus du jour, but worrisome findings about the last outbreak that shook the world are continuing to emerge. At a meeting in Boston last night, researchers presented new evidence that the Ebola epidemic in West Africa has had long-term effects on many survivors, including joint pain, neurological problems, and eye damage. They also found that many men harbor RNA from the virus in their semen after they recover and for far longer than imagined—which suggests that fresh outbreaks caused by sexual transmission are still a threat—and that many people may well have had Ebola without realizing it.
Scientists also presented disappointing results from a clinical trial of what was once considered the most promising Ebola treatment: an antibody cocktail called ZMapp. The study, started late in the epidemic, enrolled far fewer people than researchers had planned, and it failed to provide statistically significant results.
The details were revealed last night during a special session at the largest annual HIV/AIDS meeting held in North America, the Conference on Retroviruses and Opportunistic Infections. The Ebola findings were decidedly off-topic, but meeting organizers decided to make room for them because of overlap in the HIV and Ebola research communities and because of the magnitude of the epidemic.
Eugene Richardson, an infectious diseases specialist at Stanford University in Palo Alto, California, kicked off the session with data from an unusual study he helped conduct in Sierra Leone. Working with Partners in Health, a nonprofit headquartered in Boston, and Sierra Leonean researchers, Richardson went to a hard-hit village a year after the last transmission occurred. He wanted to determine how many people might have been infected without ever being diagnosed.
During the epidemic, 34 villagers had a confirmed or probable cases of Ebola. Richardson and his colleagues visited their homes and tested blood from 207 people who had lived there but weren’t known to have had Ebola. Fourteen of them had Ebola antibodies, indicating that they had been infected.
Two of these people, it turned out, had had fevers during the quarantine period, and thus would have been suspected cases if Ebola teams had found them. “We asked, ‘Where were you when we were coming around with the surveillance?’” Richardson said. “They said, ‘Hiding in the bush.’” The other 12 people with antibodies reported no symptoms at all. That means that overall, 25% of the 48 people in the village who were confirmed to have Ebola—or were deemed likely cases—had no symptoms.
Although positive antibody tests do not prove that people were infected—different diseases can trigger the production of similar-looking antibodies—other findings supported the suggestion that Ebola infections can occur without any symptoms. In a presentation about two Ebola vaccines tested in Liberia, scientists reported that 6.3% of the people who enrolled had Ebola antibodies before they received the experimental products. As Fatorma Bolay, director of the Liberian Institute for Biomedical Research, explained, these participants had “no knowledge of prior Ebola virus infections.”
“It’s certainly possible, if not likely, that there’s asymptomatic infection,” said Nancy Sullivan, an Ebola researcher at the U.S. National Institute of Allergy and Infectious Diseases (NIAID) in Bethesda, Maryland, who co-chaired the session. Smaller studies some 15 years ago from an outbreak in Gabon also reported high levels of asymptomatic infection.
The enormous scope of the epidemic of 2013–16—which sickened more than 28,000 people and killed 11,316—has allowed investigators to gather the most precise evidence ever obtained about long-term harm caused by the Ebola virus, including its uncanny ability to linger in the body after the patient recovers. Jean-François Etard of the Institute of Research for Development (INSERM) in Montpellier, France, described an ongoing study of survivors he is conducting with Guinean colleagues. To date, they have examined 475 people whose blood was deemed clear of the virus on average nearly 8 months earlier.
During clinical exams, 83% of the people reported at least one long-lasting symptom, the most common being joint or muscle pain, headaches, and fatigue. Eye exams by specialists showed abnormalities in nearly one in five patients, and two children had gone blind from cataracts. The researchers obtained semen samples from 107 men; 6% tested positive for Ebola RNA. The team found viral RNA in semen as late as 9 months after a man had been discharged from an Ebola center.
A second study provided more details on how long the Ebola virus can remain present in semen. INSERM researcher Daouda Sissoko studied 26 men in Guinea who provided samples repeatedly; 55 days after disease onset, 73% still had Ebola RNA in their semen, and at day 246—more than 8 months after they got better—27% were still positive. One man was positive at 334 days. More sobering still, a different study among 97 men in Liberia reported that one man’s semen tested positive 18 months after his recovery, and three men had Ebola-positive semen after two earlier samples had tested negative.
Positive RNA tests do not mean a person is infectious; it’s possible that the virus is no longer viable or is present in such minute quantities that it no longer poses a threat. Still, sexual transmissions from survivors deemed clear of the virus have already been documented, and the World Health Organization has urged men who have recovered from Ebola to use condoms for at least 12 months after recovering from the disease or until they have two negative RNA tests for virus in their semen. “A single sexual transmission could restart the chain of transmission,” Etard emphasized.
The session’s final presenter unveiled the much-anticipated results from a multicountry trial of ZMapp, the frontrunning experimental treatment after it rescued monkeys from Ebola a whopping 5 days after their infections occurred. NIAID’s Richard Davey, who co-led the study, explained that the trial, which recruited patients in Liberia, Sierra Leone, Guinea, and the United States, had hoped to enroll 200 people. They would either receive “optimized standard of care”—the control group—or that intervention plus three intravenous infusions of ZMapp spaced 3 days apart. In the end, the waning epidemic forced the team to end the study late last month after enrolling only 72 people.
ZMapp contains three antibodies (colored) that attach to different parts of the Ebola surface protein (gray).
ZMapp contains three antibodies (colored) that attach to different parts of the Ebola surface protein (gray).
Daniel Murin and Andrew Ward
One participant was “lost to follow up,” Davey explained, and of the remaining 71, 21 died: 37% in the control group versus 22% in those who received ZMapp. “One has to choose one’s adjectives carefully,” Davey said. “This is certainly suggestive of a trend in favor of the ZMapp containing arm.” But the results were not statistically significant.
As Science reported last month in a special report, the gigantic effort to test new drugs and vaccines in Guinea, Sierra Leone, and Liberia has produced a thin harvest; a vaccine produced by Merck is the only product that has yielded unequivocally positive results. Many held out some hope that the ZMapp study—which used a randomized controlled design, the gold standard in clinical trials—would deliver another bit of good news.
Mapp Biopharmaceutical, the San Diego, California, company that makes ZMapp, issued a press release yesterday that quoted its CEO, Kevin Whaley, saying the company will now “vigorously pursue the further development and application for licensure of ZMapp as a treatment for Ebola.”