John-Arne Røttingen, the director of the Division of Infectious Disease Control at the Norwegian Institute of Public Health and adjunct professor of Global Health and Population at Harvard University, is one of the co-authors of the successful rVSV-ZEBOV Ebola vaccine trial. He worked alongside the WHO, Wellcome Trust, the government of Canada, MSF, the London School of Hygiene and Tropical Medicine and manufacturers Merck and NewLink.
Ebola Deeply: Firstly, congratulations on such groundbreaking work. What was your reaction when you saw that the vaccine had such an extraordinary success rate?
Røttingen: I must say we were really happy and astonished with the strong results, and the fact that there were no cases among those immediately vaccinated, ten days after vaccination. This is extraordinary. Compare that to 16 cases in the other group; mathematically, it’s a vaccine that is 100 percent effective, for the time being. Of course we know that if we had conducted a much larger study, there may have been some breakthrough cases.
Ebola Deeply: You co-designed the study. Why did you choose a ring vaccination approach?
Røttingen: We did it first and foremost because we wanted to provide complementary evidence to other trials that were already planned for Sierra Leone and Liberia. We wanted to do it in a relevant public health manner. Ring vaccination seemed the most relevant approach, given the experience from smallpox eradication, and also thinking about the way in which Ebola spreads. It seemed the most relevant way to potentially use the vaccine in the future.
The trial is still ongoing. Due to the recommendation by our independent data safety management board, we made a decision to discontinue the control arm, so as of last week we decided to vaccinate all rings immediately. The study will continue in that matter and we will still get data on the effectiveness of the vaccine, but not as a randomized trial.
Ebola Deeply: Why did you decide to conduct the trial in Guinea?
Røttingen: The outbreak has been lower in Guinea than in Sierra Leone or Liberia, and it has been moving around a bit. We wanted to move with the outbreak and target high-risk individuals so that they could be provided the opportunity to benefit from a potential vaccine.
We planned to start in the Guéckédou region of Guinea, but when we were ready to go into the field, the outbreak had moved to the region around Conakry and the coastal prefectures. We have been doing vaccinations in most of the prefectures where there have been cases since March.
Ebola Deeply: The study is ongoing. Might you be able to extend the size of the vaccination ring in Guinea?
Røttingen: Currently we have been getting the vaccine from the manufacturers and we will get another shipment, so we hope that the vaccine stocks won’t be an issue. We may potentially be able to extend the size of the vaccination ring and also potentially include children and adolescents, because there is new safety data from other countries indicating that the vaccine is safe for them. They weren’t able to take part in the trial at the time. I don’t think there should be limitations on numbers and we potentially hope to vaccinate many more people.
Ebola Deeply: Pregnant women and breastfeeding mothers could not take part either. Is there any safety data that could enable them to benefit?
Røttingen: Not yet. Normally we would want larger safety studies to be conducted before vaccinating them. They are the final group to involve because of potential concerns.
Ebola Deeply: The vaccine efficacy was found to be 100 percent, but as the study says, at the cluster level, with the inclusion of all eligible adults, vaccine effectiveness was 75.1 percent. What does this mean?
Røttingen: We primarily looked for effectiveness among those who received the vaccine. The cluster level data represents the total effectiveness, or rather the indirect effectiveness, among a wider group, including among those who were not vaccinated – such as those who declined the offer, or whom we were unable to vaccinate. In that wider group we also included children, adolescents and pregnant or breastfeeding women. We found that there is some indirect effectiveness of the vaccine – that’s something we will look further into during the follow-up.
Ebola Deeply: Tell us about the safety profile of the vaccine. Does the vaccine produce any side effects?
Røttingen: The safety data is very promising. We saw some side effects during the trial, such as fever or feeling tired, but we’d expect these things with a vaccine like this. But in general, the safety profile is very good. We will look into this more as we do the longer-term follow-up.
Ebola Deeply: At this point, do you have any idea how long protection might last in vaccinated individuals?
Røttingen: It’s difficult to look at long-term protection in a study like this, but what we will keep doing is looking at how long the immune response will last, and examine the antibody level one year after immunization.
Ebola Deeply: One of the reasons why Ebola persists in Guinea and Sierra Leone is the element of fear and resistance to seek treatment. How did you decide on the best way to approach communities?
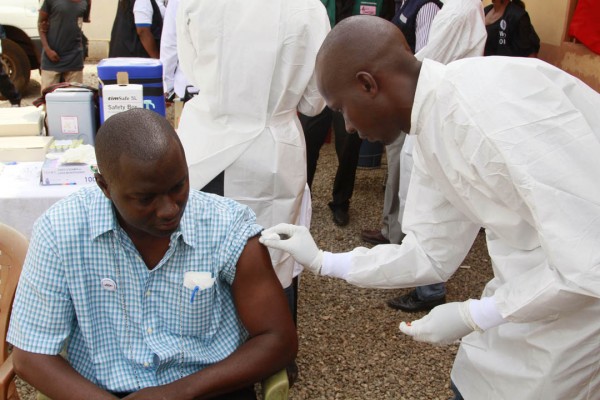
Røttingen: We invested a lot of thought into how to approach the communities in a careful manner. All of our vaccination teams are West African, many from guinea. They know the local languages and communities are approached by communicators before any vaccination team goes in. We’ve tried to profile it very much as a local response. In general that helped, and there was a positive attitude towards the trial. Of course there were a couple of communities that could not get involved, but those were very few.
Ebola Deeply: Public health experts are calling for emergency licensing. What is the process?
Røttingen: The licensing process has not been decided yet, and first and foremost it’s a decision by Merck, the manufacturer. They can decide to apply through different licensing paradigms. They can go through emergency licensing, or through the usual route. Either way, it will take several months, and most likely the vaccine won’t be ready until late this year. That’s why it’s very important to continue the trial and provide access to the vaccine within the ongoing study. Without a license, that’s the best way to make sure individuals are protected.
An extension of the trial, in Sierra Leone, could also potentially be conducted, depending on the authorities and research collaborations.
Ebola Deeply: Lastly, the public health community is documenting lessons learned during the Ebola outbreak. What has been the most significant takeaway for you?
Røttingen: There’s a long distance between theory and practice. It’s really important to strengthen capacity on the ground, so we can follow through with what is being said and learned. That also goes for trials, because without appropriate implementation, medical and vaccine trials would not be successful. I’m very impressed by the way this trial was implemented in the field, by the World Health Organization (WHO) and the West African teams there. I can say that because I’ve not been an implementer in the field. That’s what I’ve learned. I believe the way that this trial has been implemented has already contributed to the control of Ebola in Guinea.
CULLED FROM EBOLA DEEPLY
Photo by University of Oslo